DISEASE AREA
Severe postpartum haemorrhage (sPPH)
Obstetric haemorrhage is the most common and dangerous complication of childbirth.
Primary postpartum haemorrhage (PPH) is excessive bleeding within 24 hours of delivery and is the most common obstetric haemorrhage.1
- Primary PPH is typically defined as blood loss of ≥500 mL for vaginal delivery and ≥1000 mL for caesarean delivery within 24 hours of delivery.2
- Severe PPH (sPPH) a continuous blood loss of ≥1500 mL within 24 hours following delivery.3
- Secondary PPH is bleeding that occurs 24 hours to 12 weeks postpartum.4
The definition of PPH varies across international and local guidelines
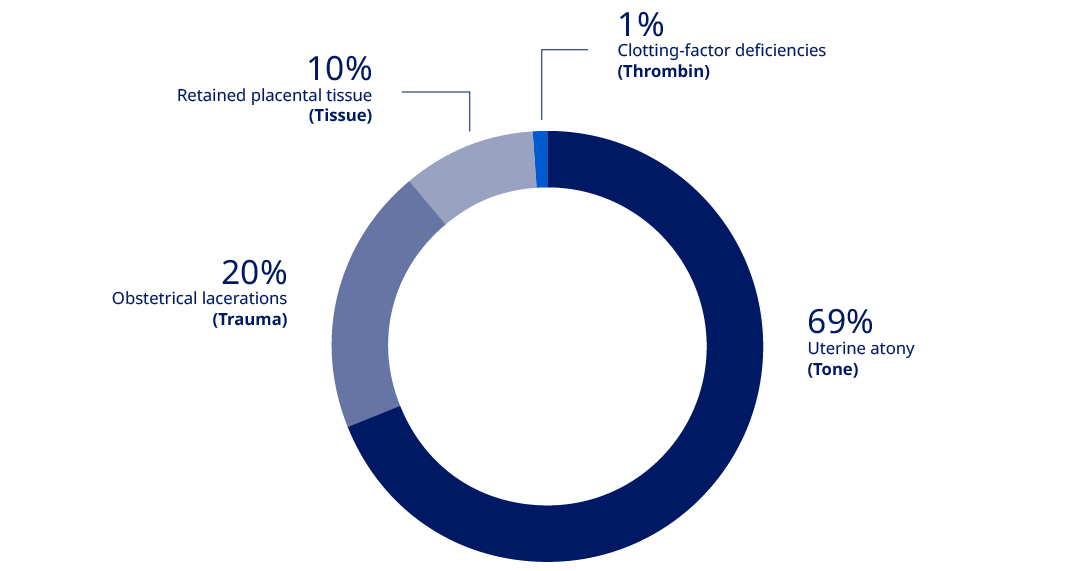
The most common cause of PPH is uterine atony followed by trauma during delivery and problems with placental positioning and delivery (e.g. placenta previa).
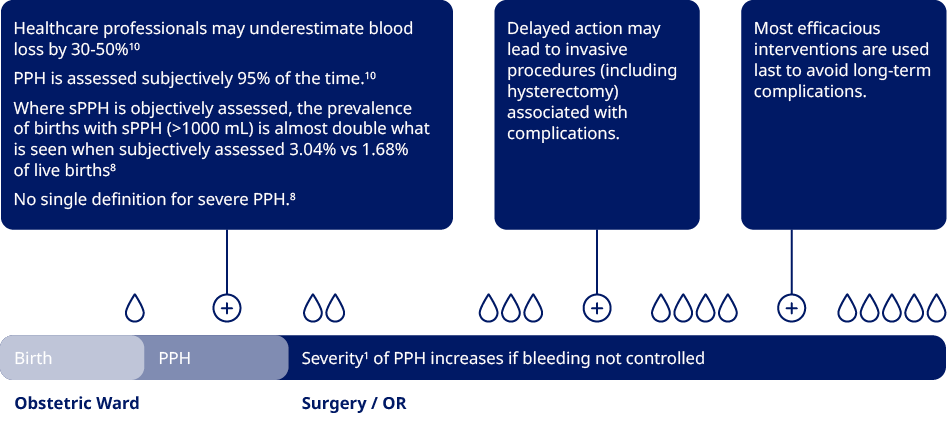
PPH is a dynamic situation, and the initial triggers can lead to the patients having multiple causes of PPH.
PPH is the leading cause of maternal illness and mortality globally.1
Worldwide, PPH accounts for
- 8% of maternal deaths in developed regions of the world.6
- 20% of maternal deaths in developing regions.7
Complications following severe PPH are often critical and can include4
- Organ failure
- Multiple organ failure
- Hemorrhagic shock
- Hysterectomy
- Loss of fertility
PPH prevalence increases with increase in birthing populations age/change
Prevalence of sPPH varies from 1.62 to over 6% of all deliveries, dependent on geography.8

Uterine atony
- Higher BMI
- Multiple pregnancy
- Older age (e.g., pregnancy after age 40)
- High birth weight (macrosomia)
- Assisted conception
- Induction of labour
Abnormal placental implantation, placenta accreta/increta/percreta
- Previous Caesarean deliveries
Severe PPH is highly prevalent (1-3% of live births in Europe1) and the #1 cause of maternal mortality.
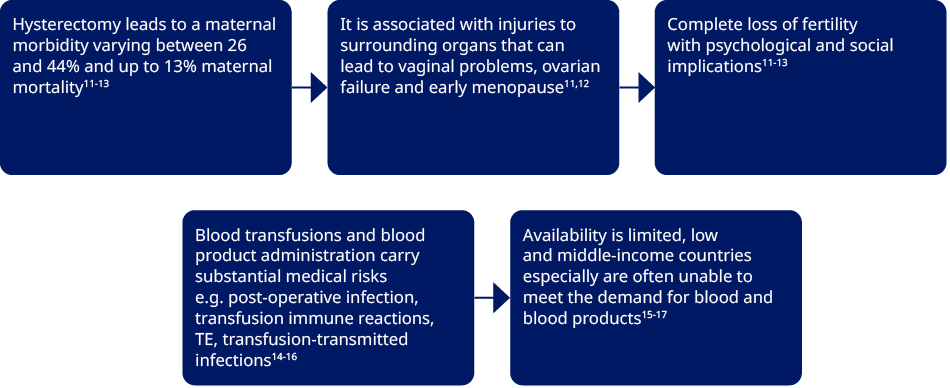
Complications following severe PPH are often critical and can include:4
- Organ failure
- Thrombo-embolic events (TE)
- Hemorrhagic shock
- Hysterectomy
- Loss of fertility
While there are known risk factors, PPH is highly unpredictable and can affect any woman.
Munoz et al. NATA consensus, Blood Transfus 2019.
Ashigbie P. Update on 2004 Background Paper, BP 6.16. 2013.
Colucci et al. Clin Appl Thromb Hemost. 2018;24(6):884-93.
Bienstock et al. N Engl J Med 2021;384:1635-45.
ACOG Practice Bulletin No. 183. Obstet Gynecol. 2017;130(4):e168-e86.
MBRRACE-UK Maternal Deaths and Morbidity 2017-2019.
Say et al. Lancet Glob Health. 2014;2(6):e323-33.
Carroli G et al. Best Practice & Research Clinical Obstetrics and Gynaecology. Vol. 22, No. 6, pp. 999–1012, 2008.
SCASMM 10th Annual Report 2012.
Glover P. Aust J Midwifery 2003;16(2)21–4; 2. (Image obtained from) Bose P et al. BJOG 2006;113(8):919–24.
Zhang et al. Medicine (Baltimore). 2017;96(45):e8443.
Christopoulos et al. J Obstet Gynaecol. 2011;31(2):139-41.
Michelet et al. Gynecol Obstet Fertil. 2015;43(12):773-9.
Sihler et al. Chest. 2010;137(1):209-20.
Taylor et al. Transfus Altern Transfus Med. 2008;10(3):112-26.
Thurn et al. Thrombosis Research 165 (2018) 54–60.
P. Ramler et al. BMC Pregnancy Childbirth. 2017;17(1):197.